Polycystic Ovary Syndrome (PCOS) is a common endocrine disorder that affects 5% to 20% of female of reproductive age worldwide. PCOS is often associated with menstrual cycle disruption, insulin resistance, high levels of androgens (like testosterone) and infertility.
While there are genetic components impacting PCOS, there is also a relationship between our gut microbiome and PCOS. In this post we are going to explore this connection further and discover the steps you can take to improve your gut health to manage PCOS.
How Do I Know if I Have PCOS?
PCOS diagnosis is not always straightforward. There are many symptoms, and there is no single test to determine if you have, or don’t have PCOS.
The signs and symptoms of PCOS can also be improved with lifestyle changes, which can ‘mask’ some of the typical features. For example, if you have very long menstrual cycles but you then start exercising regularly, your cycles may return regularly!
If you have PCOS you may experience some of the following impacts:
Feeling Hungry, Even Though You Just Ate?
It’s not about self-control – it’s about appetite hormones! PCOS can make you less satisfied and more hungry following a meal [1]. There are differences in appetite hormone regulation with PCOS that make you hungrier. Combine these changes in appetite hormones with reductions in how sensitive your body is to insulin and you can appreciate why you might be having cravings!
Insulin resistance is common in PCOS and this impacts our metabolism, making it more difficult to loose weight. Insulin resistance can also impact our fertility. You can read more about insulin and pregnancy here.
Skin Breakouts, Hair Loss or Infertility?
Hormone imbalances associated with PCOS contribute to acne, head hair falling out while you may have extra hair growing on your jawline, irregular ovulation and trouble conceiving.
These changes are all closely related to disruptions in our gut microbiome.
Individuals with PCOS often have chronic low-grade inflammation, characterised by increased circulating levels of inflammatory proteins, which leads to insulin resistance and disrupts menstrual cycle regularity. Levels of oxidative stress are also increased in PCOS [2].
Our bodies have great defences against oxidative stress which include circulating levels of Vitamin C, Vitamin E and other antioxidant enzymes. With PCOS these defences tend to be lower. Reducing inflammation and oxidative stress, and raising antioxidant defences can help restore balance [3] for better hormone balance, glowing skin and regular menstrual cycles.
You can read more about hormones and PCOS here.
Diagnosing PCOS
Diagnosis of PCOS entails meeting 2 out of the 3 following Rotterdam Diagnostic Criteria:
1. Irregular Menstrual Cycles. There can be several causes of irregular (longer than 35 days) or absent periods but a common one is PCOS. In females not ovulating regularly or having a regular menstrual cycle, their eggs are under more stress with higher levels of inflammation and oxidative stress in the fluid surrounding eggs as they mature.
Imagine if you could be ovulating regularly! Not only is this a great sign that your eggs are maturing in a healthier, happier environment and that your uterus is more receptive, but you have more opportunities for natural conception (depending on your circumstances).
Even if you are preparing for assisted fertility treatment, a regular menstrual cycle is a good indicator of better reproductive health and fertility.
2. High Androgen Levels. In females, androgens are produced mainly in the ovaries and adrenal glands. They are important for our reproductive health, muscle development and cognitive function.
Androgens you may have heard of include testosterone, androstenedione and dehydroepiandrosterone-sulfate (DHEA-S). When androgen levels are high, they stimulate the production of luteinising hormone (LH). The increased LH changes the way our follicles mature, impacting the eggs inside them.
With increased production of LH, ovulation does not occur. In combination with high androgens, the LH/FSH (follicle stimulating hormone) ratio in PCOS may be as high as 2 or 3, compared to 1 to 2 in a female without PCOS.
If you have had a blood test on day 2 or 3 of your menstrual cycle you can calculate your LH/FSH ratio by taking your LH value and dividing it by your FSH ratio. Do interpret these with a qualified practitioner as there are other factors that can influence this.
3. Polycystic Ovaries. With a transvaginal ultrasound your specialist can look at your ovaries to check their size and appearance. If your ovaries present as enlarged with multiple small follicles, this is considered as polycystic ovaries.
Some other common symptoms associated with PCOS include:
- Vitamin D Deficiency
- MTHFR gene mutation
- Sleep Disturbances
- Increased Anxiety and Depression
- High Cholesterol
Your Gut Microbiome
The community of microbes that reside in your gut provide a foundation for your reproductive health. We have over 2kg of microorganisms or microbiota living in our gut (these are mainly bacteria). These microbiota produce essential vitamins, regulate our immune system, influence our metabolism, alter hormone levels, our muscle strength and even our mood.
A healthy, diverse gut microbiome is associated with better health and wellbeing. A healthy gut is typically one many different types of microbes, and lots of them. This richness of different species and abundance (how many there are) of microbes provides a measure of diversity.

In females with PCOS gut microbiota diversity is reduced. There tends to be more species living the gut that promote inflammation and metabolic disruption, and less beneficial bacteria that help us produce beneficial compounds.
With gut dysbiosis there is an increase in androgens (hyperandrogenism) which may suppress ovulation. In females with PCOS groups of related bacteria influenced appetite, body weight, sex hormones and brain-gut communication [4].
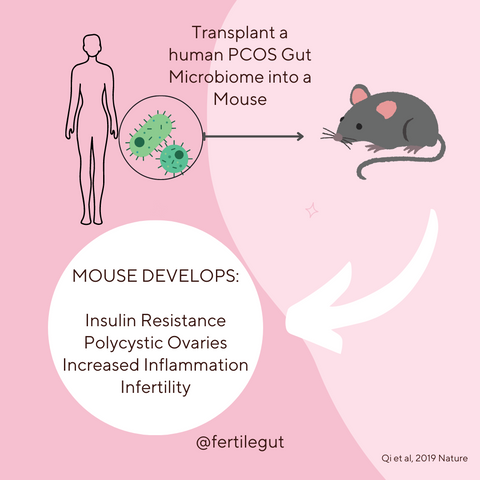
If you have PCOS, it is also likely that you have elevated levels of Bacteroides vulgatus (B. vulgatus) taking up residence in your gut [31]. When B. vulgatus are taken from the gut of a female with PCOS and transplanted into the gut of mice, these mice develop insulin resistance, increased inflammation, increased circulating endotoxin, reduced ovarian function and reduced fertility.
When mice with PCOS receive healthy human gut microbiota, the symptoms of PCOS and reduced and fertility is improved [5-8].
Your Gut Microbes and TMAO
Trimethylamine is a small, organic compound produced by your gut microbiota when it breaks down choline and carnitine. For most people, the majority of choline and carnitine in the diet comes from animal products such as pork and beef. Diets high in animal protein, and low in fibre have been associated with increased trimethylamine production by gut microbes.
Trimethylamine gets absorbed from the gut and converted to trimethylamine oxide (TMAO) which can have impacts on the health of the rest of the body. Females with PCOS have also been shown to have higher circulating levels of TMAO.
Increased TMAO has been associated with cardiovascular disease and high levels are also shown to reduce embryo quality and fertilisation [9].
Remodelling the gut microbiota is a great approach to reducing circulating TMAO. Feeding your gut bugs with plant-based proteins and reducing animal proteins is a great place to start. Plan a few meat free, plant based meals this week to nurture those microbes.
Nurture your Gut Health for PCOS
As our gut microbiome impacts PCOS, improving the diversity of the gut microbiome is an effective strategy to manage PCOS. Want more regular periods, improved fertility, and better hormone balance? It starts in the gut!
Increase Your Dietary Prebiotics
Prebiotics are essentially the ignition source for promoting the growth of beneficial bacteria in your gut. They are non-digestible, fermentable components of foods and it is likely that you have already had some today. Your gut microbiota love to break down prebiotics as a fuel source to create all the health promoting compounds that enhance your fertility.
Prebiotics may improve insulin resistance, lower androgens, and benefit lipid profile [10]. Prebiotic fibre increases beneficial gut bacteria and reduces pathogenic bacteria, reducing symptoms of PCOS.
Positive changes in the gut microbiome following prebiotic supplementation are related to reductions in circulating levels of LPS, inflammation and testosterone, while improving insulin sensitivity.
Our Microbiome Essentials formulation contains multiple prebiotics proven to nurture a diverse gut community and manage PCOS. Our Gut + Hormone delivers other supportive active ingredient proven to reduce PCOS symptoms, regulate the menstrual cycle, reduce PMS and lower androgens.
This is good news for your reproductive health!
Sleep
Sleep regulates the body’s ability to handle blood sugars by altering insulin levels, and how sensitive our bodies are to insulin. Sleep disruption can have a greater impact on insulin resistance than a high high-fat diet! One week of reducing sleep in healthy males from 10 hours in bed to 5 hours reduces insulin sensitivity by 20%.
Our transition to sleep is controlled within our brain but did you know that your gut microbiota can communicate with your brain? If you have a healthy, diverse gut microbiota levels of gut inflammation are lower and this has been shown to promote sleep.
When your gut microbota are out of balance, levels of inflammation are higher and this can hinder sleep.
A more diverse gut microbiota is positively correlated with increased sleep efficiency and total sleep time, and reduced sleep fragmentation. This means that you get to sleep quicker once your head hits the pillow, you wake less, and that because you are falling asleep quicker for the same time in bed you get more hours sleeping.
In combination with exercise, reducing stimulants like coffee in the evening and avoiding bright light from a screen, prebiotics have been shown to boost the production of neuroactive metabolites by your gut microbiota to improve sleep and stress resilience.
Move Your Body - Exercise and Your Gut Microbiome
It has been said that if you could package all the benefits of exercise into a pill that it would be the most prescribed pill in history. Who wouldn’t want to be able to increase strength and endurance, improve mood, enhance quality of life, increase energy levels, reduce body fat, increase metabolism, have better quality sleep, improve cognitive function, reduce risk of chronic disease, prolong life, improve mobility, AND enhance fertility and pregnancy success? All these benefits come with the right exercise prescription.
While diet is a potent modulator of your gut microbiome, exercise can also improve the diversity of your gut friends for optimal fertility outcomes. Exercise can increase the proportion of beneficial bacteria living in your gut, increasing production of compounds that dampen PCOS pathology and promote health and fertility. With the changes in your gut microbiome, regular exercise can restore ovulation, lower androgens and improve insulin sensitivity.
Regular aerobic exercise and strength training is a powerful combination to nurture your gut microbiome toreduce inflammation, balance hormones and boost metabolism to manage PCOS.
Your Gut-Fertility Connection
Restoring balance to your gut will set the path to reduce inflammation and oxidative stress, restore hormone balance, regulate your immune system, enhance your metabolic health, increase resilience and optimise your reproductive health.
Address your Fertility at the Foundation and Nurture Your Gut Microbiome!
References
- 1. Moran, L.J., et al., Ghrelin and measures of satiety are altered in polycystic ovary syndrome but not differentially affected by diet composition. J Clin Endocrinol Metab, 2004. 89(7): p. 3337-44.
- 2. Mohammadi, M., Oxidative Stress and Polycystic Ovary Syndrome: A Brief Review. Int J Prev Med, 2019. 10: p. 86.
- 3. Fatima, Q., et al., Evaluation of antioxidant defense markers in relation to hormonal and insulin parameters in women with polycystic ovary syndrome (PCOS): A case-control study. Diabetes Metab Syndr, 2019. 13(3): p. 1957-1961.
- 4. Liu, R., et al., Dysbiosis of Gut Microbiota Associated with Clinical Parameters in Polycystic Ovary Syndrome. Frontiers in Microbiology, 2017. 8(324).
- 5. Chappell, N.R., et al., Hyperandrogenemia alters mitochondrial structure and function in the oocytes of obese mouse with polycystic ovary syndrome. F S Sci, 2021. 2(1): p. 101-112.
- 6. Crunkhorn, S., Role of the gut microbiota in PCOS. Nat Rev Drug Discov, 2019. 18(9): p. 668.
- 7. Guo, Y., et al., Association between Polycystic Ovary Syndrome and Gut Microbiota. PLoS One, 2016. 11(4): p. e0153196.
- 8. Qi, X., et al., The impact of the gut microbiota on the reproductive and metabolic endocrine system. Gut Microbes, 2021. 13(1): p. 1-21.
- 9. Nagy, R.A., et al., Trimethylamine-N-oxide is present in human follicular fluid and is a negative predictor of embryo quality. Human reproduction (Oxford, England), 2020: p. dez224.
- 10. Kim, Y.A., J.B. Keogh, and P.M. Clifton, Probiotics, prebiotics, synbiotics and insulin sensitivity. Nutr Res Rev, 2018. 31(1): p. 35-51.